Treating Xanthelasma: Cholesterol Deposits Around the Eyes

Small yellow bumps or patches along the eye lids are often dismissed as harmless blemishes or growths, but they can have a deeper meaning. These soft, flat plaques, known as xanthelasma, form when cholesterol deposits build up under the skin. While they are benign and painless, the appearance of these deposits can be visually distressing and, in some cases, may point to an underlying lipid imbalance.
What Is Xanthelasma (Cholesterol Deposits on the Eyes)?
Xanthelasma palpebrarum refers to small, yellowish cholesterol deposits that develop just beneath the skin of the eyelids, typically near the inner corners of the eyes or along the upper eyelids. These bumps are a type of xanthoma; a term used for cholesterol-rich growths that can appear on different parts of the body.
Xanthelasma is benign, meaning it does not pose a health risk or affect vision. However, because of their high visibility (especially their yellow color), many patients seek removal for cosmetic reasons. Understanding its cause can also provide valuable insight into one’s cardiovascular health.
Symptoms and Appearance
Xanthelasma is easy to recognize once you know what to look for:
- Texture: Typically soft, flat, or slightly raised plaques under the thin eyelid skin.
- Color: While color varies, most instances fall between pale yellow to orange, sometimes blending with surrounding skin.
- Location: Often manifesting symmetrically on both eyelids, most often near the inner corners by the nose.
- Progression: Lesions grow slowly over time and may merge to form larger patches.
Xanthelasma deposits are usually painless and non-itchy, though they may become more noticeable as they expand.
Is Xanthelasma Harmful to One’s Health?
On its own, xanthelasma is not dangerous and will not affect your vision or eye function. However, its presence can signal an imbalance in the body’s fat metabolism.
Studies show that up to 50% of people with xanthelasma have elevated cholesterol or triglycerides (1). Since these lipid abnormalities increase the risk for cardiovascular disease, it is wise to treat xanthelasma as an early warning sign. Patients are advised to discuss Xanthelasma with their primary care physician. A lipid panel and heart-health assessment can determine whether additional management is needed.
What Causes Xanthelasma?
Xanthelasma forms when cholesterol builds up inside skin cells called macrophages. Over time, these lipid-filled cells cluster in the eyelid tissue and create visible yellow plaques.
Several underlying factors can contribute to this process:
- High LDL (“bad”) cholesterol or elevated triglycerides
- Liver or metabolic conditions, such as fatty liver disease or hypothyroidism
- Inherited lipid disorders like familial hypercholesterolemia
- Chronic inflammation or minor trauma to delicate eyelid skin
However, it is important to note that even individuals with normal cholesterol levels can develop xanthelasma, suggesting that genetics and local skin changes play a role as well.
Who Is More Susceptible to Developing Xanthelasma?
Xanthelasma typically affects adults between 30 and 60 years old and is more common in women than men. It’s seen more frequently among individuals of Asian or Mediterranean descent, though people of any ethnicity are susceptible to Xanthelasma development.
Risk factors common to people with Xanthelasma include:
- Elevated cholesterol or triglycerides
- Diabetes, obesity, or metabolic syndrome
- Family history of high cholesterol or lipid disorders
- Smoking or diets high in saturated fats
Are There Ways to Prevent Xanthelasma?
While genetics cannot be changed, certain habits can help reduce the risk of developing xanthelasma, or prevent new spots after treatment:
- Monitor cholesterol levels: Regular lipid testing allows for early detection of imbalance.
- Follow a heart-healthy diet: Choose fruits, vegetables, whole grains, lean proteins, and omega-3-rich foods while limiting saturated fats.
- Exercise regularly: Physical activity helps improve circulation and regulate blood lipids.
- Avoid smoking and limit alcohol: Both contribute to vascular and metabolic stress.
- Manage health conditions: Keep diabetes, thyroid disorders, and high blood pressure under control.
- Protect your eyelids from sun exposure: Sunglasses or SPF-formulated eye creams can maintain skin health and reduce irritation.
Will Xanthelasma Go Away on Its Own?
Unfortunately, xanthelasma rarely resolves on its own without intervention. Once cholesterol deposits form, they tend to persist or slowly enlarge over time.
Lifestyle changes, specifically health habits that lower cholesterol levels, can help prevent new lesions but will not address existing ones. Since xanthelasma is benign and not considered harmful to one’s health, treatment is primarily cosmetic and often not covered by medical insurance. However, medical evaluation is always recommended to check for underlying lipid issues.
Treatment Options for Xanthelasma
Treatment focuses on removing visible plaques while preserving the delicate eyelid skin. The best approach depends on the size, depth, and number of lesions, as well as your skin type and healing tendencies.
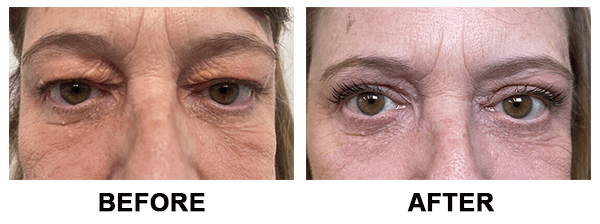
Xanthelasma Removal Surgery
Surgical excision under local anesthesia is one of the most effective options for addressing xanthelasma. The dermatologist or oculoplastic surgeon carefully removes the cholesterol bumps and sutures the area for minimal scarring. Surgery offers high effectiveness and allows excised tissue to be examined under a microscope if needed. Xanthelasma removal can also take place during an eyelid surgery (blepharoplasty) procedure.
Liquid Nitrogen (Cryotherapy)
Cryotherapy freezes cholesterol-laden cells using controlled cold exposure. After exposure, the treated skin crusts, and peels away within days. Removal via cryotherapy is quick and non-invasive but carries a higher risk of pigment change on thin eyelid skin, particularly in those with darker skin complexions.
Laser Treatment
Modern laser treatments can precisely vaporize cholesterol deposits layer by layer. This method minimizes bleeding, reduces downtime, and is ideal for small to moderate xanthelasma bumps. Healing is typically smooth with minimal scarring when performed by an experienced specialist.
Chemical Peels
Chemical peels using trichloroacetic acid (TCA) or similar solutions can gradually dissolve superficial deposits. While being affordable and non-surgical, effectively treating xanthelasma may require multiple sessions. This option is also limited to treating minor forms of xanthelasma. Mild redness or flaking is expected during recovery.
What to Expect After Treatment
Recovering from xanthelasma removal is typically a simple process, with most patients being able to fully return to normal activities within a week of treatment.
Depending on which treatment is performed, individuals can expect mild redness, swelling, or tenderness for several days following removal. Patients may be directed to keep the area clean, avoid makeup or harsh products, and apply a soothing ointment to the treatment area. Sun protection post-procedure is crucial, freshly treated skin is more prone to pigmentation.
Can Xanthelasma Come Back After Removal?
Unfortunately, recurrence of xanthelasma is possible, especially if cholesterol levels stay elevated. Factors influencing recurrence include:
- Type of removal treatment performed: Surgical or laser removal options have the lowest recurrence rates, while others feature higher chances of recurrence.
- Cholesterol and triglyceride control: Persistently high lipid levels encourage new deposits. This is why its essential for patients to take steps to lower their cholesterol.
- Genetic predisposition: Some individuals are more prone to xanthelasma recurrence regardless of lifestyle factors.
To reduce recurrence risk:
- Maintain healthy lipid levels through diet, exercise, and prescribed medications.
- Schedule regular lipid panels and medical follow-ups.
- Protect and care for eyelid skin, avoid rubbing, trauma, or excessive sun exposure.
Skincare and Eyelid Care After Treatment
Following removal, proper aftercare that focuses on gentleness is essential to ensure optimal healing and minimize the risk of discoloration. Patients should:
- Keep the area clean and moisturized with a fragrance-free ointment or gentle balm.
- Avoid rubbing, scratching, or applying pressure to healing skin.
- Use sunscreen or wear sunglasses to protect from UV damage.
- Pause use of retinoids, exfoliants, or acids until cleared by your provider.
- Monitor for any new yellowish spots. Early treatment can prevent them from spreading.
Sources
- Al Aboud A. M., Shah S. S., Blair K., Al Aboud D. M. “Xanthelasma Palpebrarum.” StatPearls [Internet], StatPearls Publishing, Treasure Island (FL), updated 1 March 2024. Bookshelf ID: NBK531501. https://www.ncbi.nlm.nih.gov/books/NBK531501/
Disclaimer: The contents of the Westlake Dermatology website, including text, graphics, and images, are for informational purposes only and are not intended to substitute for direct medical advice from your physician or other qualified professional.
Great before and after result, thanks for this post!